AIIMS, Metabolic Surgery (Credit: OpenAI )
The procedure falls under metabolic or bariatric surgery. It alters the digestive tract path. Food bypasses the duodenum and goes straight to the lower intestine. This change reportedly improves insulin sensitivity sharply. Surgeons performed the surgery on 30 patients. The procedure lasted around two hours. It is similar to weight-loss surgeries but used here to tackle diabetes directly.
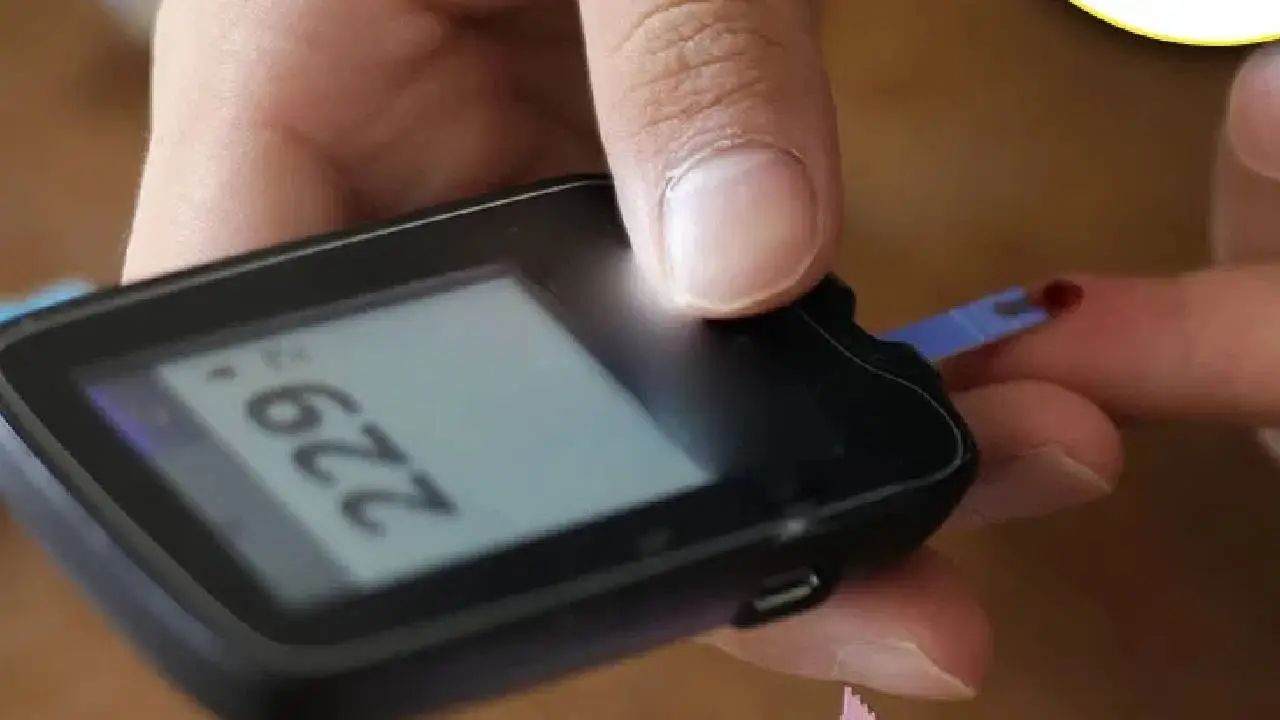
Doctors claim that almost immediately after surgery, insulin response improved. Within days, patients’ blood glucose levels reportedly normalized. Many saw their HbA1c and fasting glucose drop into safe ranges. Importantly, they no longer needed daily diabetes medication. Regular diet adjustments and healthy habits were advised. Follow-ups are ongoing to confirm long-term results. Early data appears promising.
According to the medical team, this operation benefits only type-2 diabetes. Genetic type-1 diabetes patients won’t benefit because their pancreas cannot produce insulin. The surgery aims to improve insulin sensitivity and restore pancreatic function—not address genetic deficiency. Doctors stress that claim applies strictly to adult-onset type-2 cases. Patients must undergo screening to see if they qualify.
As with any surgery, risks exist. Infection, nutritional deficiencies, and lifestyle adjustment challenges remain. Post-op diet must be managed strictly. Long-term success partly depends on patient compliance with healthy food and exercise. Doctors warn that if lifestyle habits decline, diabetes symptoms could recur. Regular monitoring of sugar levels and overall health is recommended. Success is not guaranteed without discipline.
Dr. Manjunath, from the surgery department, said publicly: “We have patients whose sugar levels are normal without medicine.” He added that when drugs failed to control sugar, this surgery offered life-saving relief. The team believes metabolic overhaul—not just symptom suppression—can target root causes. They presented results of 30 cases to colleagues and awaiting peer-reviewed publication. Official claims still need validation by larger studies.
Several endocrinologists urge caution. They acknowledge that metabolic surgery can improve insulin sensitivity, but call for longer follow-up. They remind that diabetes is a multifactorial disease. Surgery may help some, but comprehensive care and lifestyle matter most. They worry public may view surgery as a quick fix. Standard treatments and prevention — diet, exercise, regular checkups — remain essential. Peer-reviewed evidence still awaited.
Patients with type-2 diabetes considering this surgery should consult certified specialists. They must assess risks and benefits thoroughly. Lifestyle change commitment is key. Patients should check long-term follow-up data when available. Until broader studies confirm results, medications and standard treatment remain important safeguards. Transparency, realistic expectations, and medical guidance are crucial before undertaking such surgery.





Copyright © 2026 Top Indian News
